|
Dr. Don Stader, MD, FACEP, FASAM- Keynote
Don Stader is a board-certified emergency and addiction medicine physician, opioid & pain expert, film producer, and social entrepreneur. He is a nationally recognized leader in addressing the opioid crisis, pain management, medication for addiction treatment, and harm reduction.
Don is a Co-Founder and CEO of Epifluence, and also serves as the Medical Director of the Compass Opioid Stewardship Program, Medical Director of Colorado ROOTS, and Executive Director of The Naloxone Project. Don has decades of experience in leadership, innovation, and creative arts. He has served as President of the Emergency Medicine Residents' Association and COACEP. Don has founded 3 nonprofits, including the Naloxone Project, Advanced Analgesia, and the Emergency Medical Minute. In regards to hospital and medical leadership, he is the previous Section Chair of Emergency Medicine at Swedish Medical Center, and the previous Senior Pain Management & Opioid Policy Physician Advisor to the Colorado Hospital Association. Don practices Emergency and Addiction Medicine at Lincoln Health in Hugo, CO.
Don's creative works include the Emmy-winning documentary 24/7/365- The Evolution of Emergency Medicine, Emmy-nominated Dying in your Mother's Arms, and film Palliative. He has produced 2 books, serving as the Editor-in-Chief of Bring EM' All and Advanced Analgesia in the ED. He has served as Editor-in-Chief of multiple medical guidelines addressing the opioid crisis.
He lives with his wife Andi and their three daughters Josiphine, Audrey & Morgan and dog Pepper in Denver, Colorado.
|
|
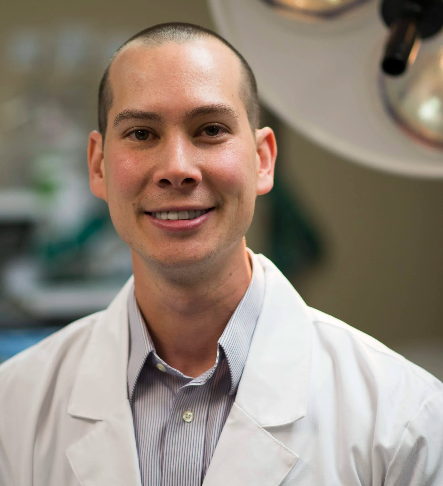
Josh Blum, MD
Joshua Blum is a primary care internal medicine and addiction medicine doctor in Denver, Colorado. He teaches locally and nationally on pain management, opioid stewardship, and substance use disorder identification and treatment.
|

|
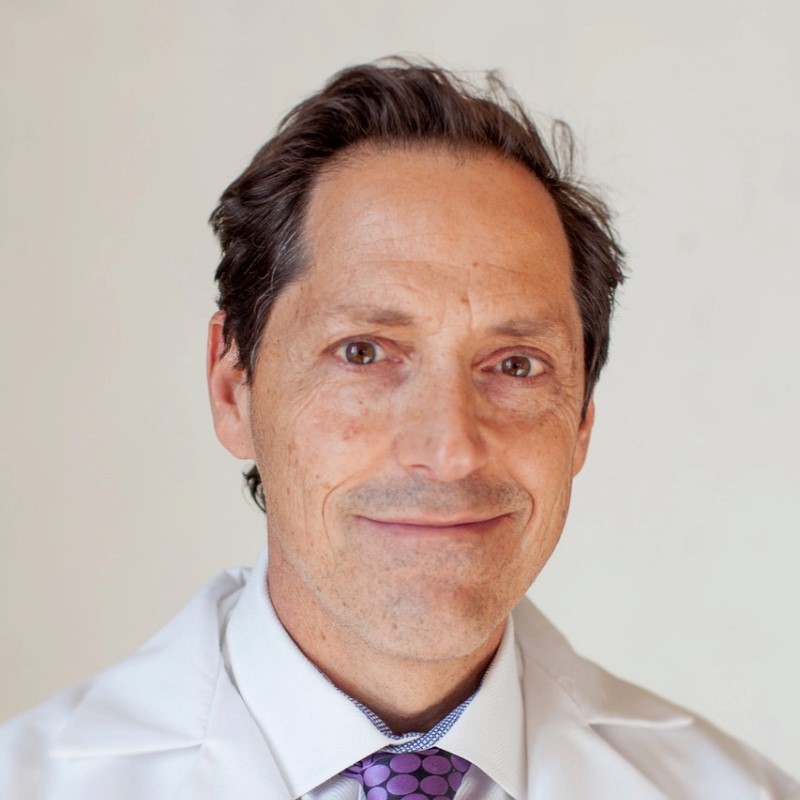
Scott Weiner, MD, MPH, FAAEM, FACEP, FASAM
Scott Weiner, is an Associate Professor of Emergency Medicine at Harvard Medical School and the McGraw Endowed Chair in the Department of Emergency Medicine at Brigham and Women’s Hospital. He completed his emergency medicine residency at Beth Israel Deaconess Medical Center and earned a Master of Public Health from the Harvard School of Public Health. Board-certified in both emergency medicine and addiction medicine, Dr. Weiner is a nationally recognized, tech-minded researcher focused on the prevention and treatment of substance use disorders, with more than 135 peer-reviewed publications. His work emphasizes the use of technology, data, and health systems innovation to improve patient care and scale evidence-based interventions. He is deeply engaged in health policy and physician leadership, and previously served as President of the Massachusetts College of Emergency Physicians.
|

|
Rachael Duncan, PharmD, BCPS, BCCCP
Rachael Duncan is a Colorado-based clinical pharmacist who is board certified in pharmacotherapy and critical care pharmacy. She has spent the past decade focused on policy, advocacy, and educational work surrounding opioid stewardship and addiction treatment at both the state and national level. Rachael earned her PharmD from Ohio Northern University in 2011 and completed a critical care residency at Duke University hospital in 2013. She is the author and editor of multiple state- and nation- wide opioid stewardship and alternatives to opioids (ALTO) guidelines, championed the nation's 2nd emergency department (ED) ALTO program, and published the first peer-reviewed paper on ALTOs in the ED.
Previously, Rachael was a consultant for the consulting firm Stader Opioid Consultants. Prior to that, she held several clinical and leadership roles at Swedish Medical Center in Englewood, Colorado.
Rachael is the Associate Director of The Naloxone Project (TNP), a nonprofit aimed at making hospitals into naloxone distribution sites. She is also Program Director of MOMs+, a quality improvement program that partners with several state perinatal quality collaboratives, aimed at helping birthing hospitals build addiction treatment infrastructure for perinatal patients. Her current clinical practice is in rural hospital-based pharmacy.
Rachael lives in a small mountain town in Colorado with her husband and two young sons, where they enjoy biking, rafting, and skiing.
|

|
Susan Bradley, PharmD, JM
Susan Bradley is a clinical pharmacist based out of the Northern, New York area.
She is passionate about health systems and improving population health, through clinical consulting and legislative reform.
Susan earned her PharmD degree from Albany College of Pharmacy and Health Sciences in 2014, and received her Juris Master degree with a concentration in Healthcare Regulation in 2024, from Florida State University College of Law.
She holds certifications in pain management and emergency medicine through ASHP. In 2019 she completed a Healthcare Leadership Advancement Certification through Cornell University, which included a capstone project on Expanding Pharmacist Services to the Emergency Department of a rural critical access facility.
Previously, Susan worked with substance use disorder patients within the emergency department and inpatient withdrawal management (“detox”) unit, as well as supported outpatient settings. She is experienced in developing order sets for substance use disorders, leading an opioid stewardship program and writing ALTO guidelines for the emergency department. Her experience spans pharmacy leadership, clinical project development, regulatory compliance, accreditation, policy writing and systemization.
Susan's clinical practice is through Rochester Regional Health.
In her free time, Susan loves spending time with her husband, Chris, and young daughters, Amelia and Abigail. They enjoy boating and jet-skiing in the 1000 islands region where they live, as well as traveling whenever they have the opportunity!
|

|
Christine Blake Smith, D.O.
Christine Blake Smith is a quadruple board-certified physician in Addiction Medicine, Family Medicine, Lifestyle Medicine, and Osteopathic Manipulative Treatment, with over 20 years of experience in private practice.
She is one of six nationally selected clinical coaches working within a Medicare-funded opioid stewardship program, where I train the highest opioid prescribers across the U.S. in safe, patient-centered controlled-substance prescribing, opioid tapering, and risk reduction.
Her professional focus is helping clinicians increase patient safety, improve retention, and reduce regulatory and legal exposure, without abandoning patients or practicing fear-based medicine.
In parallel, she maintain a successful family and preventive care practice and develop patient-facing educational programs focused on disease prevention, behavior change, and self-healing strategies grounded in evidence-based medicine.
She the creator of the HUMOR Method™, a relationship-based, micro-change framework used in opioid stewardship, deprescribing, and patient engagement. I am also an author and national speaker for CME events, hospital systems, and professional organizations.
|